Type 2 Diabetes in Children Peer Review Sources
- Enquiry article
- Open Access
- Published:
In search of quality bear witness for lifestyle direction and glycemic control in children and adolescents with type 2 diabetes: A systematic review
BMC Pediatrics volume 10, Commodity number:97 (2010) Cite this article
Abstract
Background
Our purpose was to evaluate the impact of lifestyle behavior modification on glycemic control among children and youth with clinically defined Type 2 Diabetes (T2D).
Methods
Nosotros conducted a systematic review of studies (randomized trials, quasi-experimental studies) evaluating lifestyle (diet and/or physical activeness) modification and glycemic control (HbA1c). Our data sources included bibliographic databases (EMBASE, CINAHL®, Cochrane Library, Medline®, PASCAL, PsycINFO®, and Sociological Abstracts), transmission reference search, and contact with study authors. Two reviewers independently selected studies that included any intervention targeting diet and/or physical activity alone or in combination as a means to reduce HbA1c in children and youth under the historic period of eighteen with T2D.
Results
Our search strategy generated iv,572 citations. The bulk of citations were not relevant to the study objective. One written report met inclusion criteria. In this retrospective study, morbidly obese youth with T2D were treated with a very low saccharide diet. This unmarried study received a quality index score of < eleven, indicating poor study quality and thus limiting confidence in the study's conclusions.
Conclusions
At that place is no high quality evidence to advise lifestyle modification improves either short- or long-term glycemic control in children and youth with T2D. Additional research is conspicuously warranted to ascertain optimal lifestyle behaviour strategies for young people with T2D.
Groundwork
Globally, the prevalence of Type two Diabetes (T2D) in the pediatric population is increasing, about notably amid xv - 18 year olds [ane–4]. At diagnosis, most boys and girls with T2D are overweight or obese, have a positive family history of T2D, are peri- or mail service-pubertal, and present with metabolic risk factors (e.g., dyslipidemia) [5]. With the early on onset of this chronic condition and the associated co-morbidities, a life-long reduction in quality of life and premature mortality due to micro- and macro-vascular complications can be expected [6]. To accost this health claiming resulting from pediatric T2D, constructive and efficient management strategies are necessary.
Potent evidence supports the function of lifestyle modification to forestall (or at least delay) T2D in adults [7–11]. On this basis, many current clinical practice guidelines for adults with T2D recommend lifestyle modifications that include improving dietary quality equally well as increasing the quantity and quality of physical activity to promote weight management and improve glycemic control [12–xiv]. Electric current handling guidelines for children and youth with T2D do non differ from adult recommendations. Amongst children and youth who are asymptomatic (i.east., costless of polyuria, polydipsia, or ketoacidosis) at diagnosis, intensive lifestyle counseling is recommended to accomplish practiced glycemic control (i.e., HbA1c < 7.0% or fasting plasma glucose < half-dozen.six mmol/L) within 3 to 6 months [13–17]. If this clinical target is not achieved, initiation of metformin, an oral hypoglycemic agent, is recommended; in some cases, insulin therapy may too be necessary [xvi, 18].
Although at that place is lilliputian data currently bachelor on treatment patterns for children with T2D, it appears most boys and girls with T2D are treated pharmacologically [12]. It is non known whether this is a reflection of poor adherence to lifestyle modifications in children and youth or because clinicians' perceptions of and experiences with lifestyle recommendations and interventions are less constructive for managing T2D in this population. To address this cognition gap, we conducted a systematic review to evaluate the affect of lifestyle behavior modification on glycemic control among children and youth with clinically defined T2D.
Methods
Literature Search Strategy
A research librarian, with input from the research team, adult and implemented a comprehensive search strategy in selected loftier-yield electronic databases (EMBASE, CINAHL®, Cochrane Library, Medline®, PASCAL, PsycINFO®, and Sociological Abstracts) from their date of inception until October 2007. An updated search was completed in May 2009 (See Additional file1 for search terms). Relevant articles were also sought past searching the reference lists from manufactures retrieved for detailed review as well equally related review articles published from Jan 2002 onward. Personal contact was established with content experts and authors of selected review manufactures to ensure relevant publications were not missed. No language restrictions were applied in this search strategy.
Study Inclusion and Pick Criteria
Nosotros included all studies designed to evaluate the bear upon of lifestyle modification (diet and/or physical activity) on glycemic command (HbA1c) in children or youth with T2D. Lifestyle modification and glycemic command amidst children and youth with impaired glucose tolerance or impaired fasting glucose were non included. Similarly, the use of anti-diabetic drug therapies was not formally assessed. However, if a lifestyle modification group was included in whatever report design, the data were considered for inclusion. Studies were excluded if they did not include a comparison grouping or were not relevant to children and youth.
Two reviewers (STJ and MC) independently reviewed all abstracts and references. Studies were included if they met the post-obit criteria: original research, participants ≤18 years of age with T2D, evaluated the effect of lifestyle modification (diet and/or concrete activity) on glycemic control (HbA1c). Inter-observer agreement for study inclusion was high (κ = 0.92). Once the initial review was complete, a tertiary investigator (GDCB) resolved any discrepancies by consensus.
Quality Cess
Assessment of the methodologic quality of included studies was completed using criteria from Downs and Black [19], which assessed report characteristics including internal and external validity, power, and reporting. A maximal quality alphabetize (QI) score was given to selected studies. A QI score >20 rated good, eleven to 20 rated moderate and <eleven rated poor [19]. Ii reviewers (STJ and MC) independently completed quality assessments of included studies. Any discrepancies were resolved through 3rd party word (GDCB).
Results
Figure 1 shows the selection process for this systematic review. From the 4,572 publications identified by reviewing titles and abstracts, 61 manuscripts were selected for complete review. Of these manuscripts, 19 review manufactures were identified and removed. Additionally, seven cohort studies [20–26] and one case-written report [27] were identified and reviewed because they were closely related to our inquiry question, but did non fully match our inclusion criteria (Table 1). The accomplice studies mainly described treatment trajectories, behavioral characteristics, illness direction strategies, or quality of life among children and youth with T2D; notwithstanding, they lacked a defined lifestyle intervention or comparator group. Although the identified case-study included a specific lifestyle intervention for i child with T2D, it was excluded based on the nature of the study design. One other study [28] described the evaluation of a community-based plan that focused on nutrient preparation skills, but did non include behavioral or clinical outcomes (Table 1). No boosted studies were identified through our exam of study reference lists. Contact with experts in the field of pediatric T2D yielded ii additional manuscripts, simply upon review, these studies did not satisfy our inclusion criteria. In the end, i report (a retrospective, case-control design) met our inclusion criteria [29].
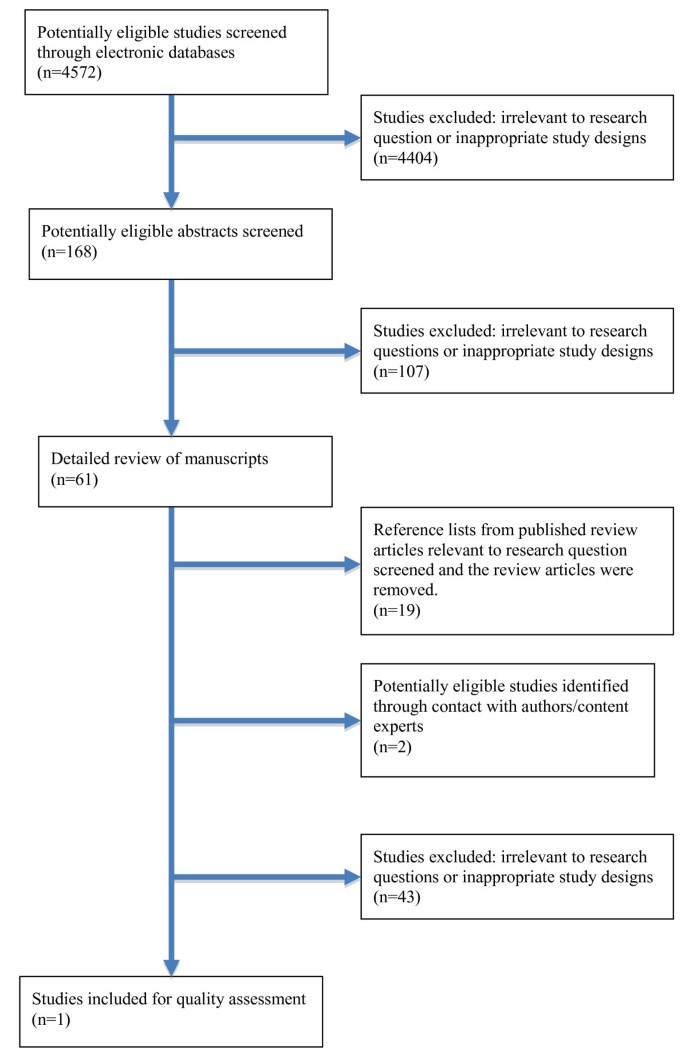
Flow diagram of systematic search.
In the study past Willi et al., [29], the apply of a very depression carbohydrate diet in the treatment of T2D was found be an constructive short-term therapy. However, this written report was of poor methodological quality and its results should exist interpreted with caution. The results are at high run a risk for bias because it was a convenience sample of hospital-based patients and was not a prospective design with random assignment to handling and control. This written report received a QI score of <11 (rated poor); additional details of this study are described in Table 2.
Discussion
Electric current treatment guidelines land that children and youth with T2D should receive intensive lifestyle counseling to assistance them achieve target glycemia within 3 - 6 months following diagnosis [12–16]. Despite this recommendation, our review of the literature revealed only i report that targeted lifestyle modification (diet) as an approach for improving glycemic command in this population. To date, most published studies have either included adults exclusively or have been based on retrospective or cross-sectional accomplice studies of boys and girls with insulin resistance, only without T2D. Our review did non reveal any high quality studies that included physical activity interventions to better curt- or long-term glycemic control in children and youth with T2D, nor did it uncover any studies that examined the influence of combining diet and physical action in the treatment of pediatric T2D. While nosotros identified many review articles concerning the management of T2D in this population, none offered new information regarding the efficacy or effectiveness of lifestyle management for glycemic control.
The lack of published studies of lifestyle direction for pediatric T2D may reflect the relatively low prevalence of the disease. Despite some having described pediatric diabetes to be at 'epidemic levels' [xxx–32], others argue prevalence estimates are of modest business organisation, even amid those populations believed to be at greater risk [33]. Nevertheless, current prevalence estimates of overweight and obesity are cause for concern with respect to the potential for developing T2D and suggest a need for evidence-based recommendations for those who have already been diagnosed and those at high risk.
The Diabetes Prevention Program [7] and other lifestyle interventions for adults at high risk for T2D [eight, 9] have provided a model for clinicians and researchers upon which to base the design, commitment, and evaluation of clinical trials for T2D management. Indeed, these studies have informed the pattern of a recently-launched T2D management trial, which includes a lifestyle component [34]. However, it is important to bear in heed that pediatric and adult populations rarely receive similar therapies in enquiry or clinical settings due to distinct metabolic, physical, developmental, and cognitive differences. Moreover, within the context of pediatric behavior modification, consideration of the complex interrelationships between environmental factors (i.e., family, peers, school, media, built environs) must be taken into account. Therefore, circumspection must be exercised when generalizing the clinical findings from currently available adult data to the pediatric population.
Of additional importance is the selection of appropriate study outcomes amongst the pediatric population [35]. Although good glycemic command and good for you trunk weights are of clinical importance, the antecedents of these clinical outcomes may be more salient [36]. For example, parental interactions with their sons and daughters when making family lifestyle changes accept a meaningful touch on [37] to the extent that the way with which parents communicate with and set boundaries within their family has considerable influence on children'south diet and concrete action behaviours [38]. In this regard, evaluating outcomes such as parenting style, self-efficacy, and motivation to change lifestyle behaviours tin can help to contextualize nutrition and physical activeness behaviours besides as metabolic outcomes that are influenced by lifestyle. Moreover, the current evidence-base for weight management may not exist a suitable proxy for programs for pediatric T2D since many of the gimmicky studies of pediatric weight management accept been carried out on pre-adolescent children from primarily Caucasian, middle socioeconomic families. The current cohort of pediatric T2D patients includes (primarily) less flush families of minority ethnic/racial backgrounds equally well as families living with generations of chronic affliction and co-morbidities of diabetes for which the disparities in health outcomes are well known in the adult T2D population.
Children and youth with T2D are unremarkably overweight or obese [17]. Electric current pediatric and adult literature provides proficient evidence for reducing free energy intake and increasing energy expenditure to enable weight direction and reduce the risk of T2D. In adults, however, weight loss is not e'er necessary to improve glycemic command [39]. Until more show is bachelor, it remains unknown whether glycemia tin exist improved in children and youth with T2D independent of weight loss. All the same, factors that can impact the accomplishment and sustainability of salubrious lifestyle changes are increasingly beingness characterized. For example, a comprehensive health assessment prior to intervention enrolment would enable the design of interventions that are tailored to the needs of individuals and families, an advancement that can optimize outcomes in sub-groups with similar features. Weight management interventions that customize treatment based on loss of command eating [xl], melanocortin iv receptor cistron mutation [41], maternal mental wellness [42], and/or motivation [43] could maximize individual responsiveness to weight management therapies. This degree of sophistication represents a substantial improvement beyond traditional variables (i.e., age, gender, obesity condition) that, to engagement, have determined study inclusion and intervention approaches. This would also provide a degree of intervention composure that moves across a 'one size fits all' for managing T2D.
Presently, the U.Southward. National Found of Diabetes and Digestive and Kidney Diseases (NIDDK) is supporting a number of large-scale, multi-center trials designed to forbid or treat T2D in children and youth under the collaborative titled Studies to Treat Or Prevent Pediatric Type ii Diabetes (STOPP-T2D). This partnership focuses on treating adolescents already diagnosed with T2D [34] and on the chief prevention of T2D among middle-schoolhouse aged youth [44]. Unfortunately, post-obit the completion of the NIDDK sponsored trial (Treatment Options for type 2 Diabetes in Adolescents and Youth: TODAY) [34], the contained effects of the dietary and physical action behavioural changes on glycemic control will remain unknown; the trial does not include an independent lifestyle modification arm. Nonetheless, trials such as these are urgently needed to inform clinical practice.
The strengths of this study include the systematic, comprehensive and unbiased approach. The results of our systematic review should however exist viewed in calorie-free of several limitations. An intrinsic limitation of any systematic review is the potential for publication and selection bias. We admit this methodological drawback and undertook manual searches and contacted recognized experts in pediatric endocrinology. This strategy did not yield whatsoever additional unpublished articles that satisfied our inclusion criteria, so it is unlikely that we missed whatsoever relevant articles.
Conclusion
In summary, our systematic review indicated that no well-designed studies have evaluated the touch on of lifestyle modification on glycemic command in children and youth with T2D. Numerous review articles take been published in this area, but contribute picayune to our show base. Randomized clinical trials must exist performed to conspicuously plant the part of nutrition and concrete activity interventions in managing pediatric T2D. These studies might besides help to determine the optimal lifestyle treatment approaches for good glycemic command contained of pharmacologic therapy for the pediatric T2D population. We believe that research to examine lifestyle-based therapies, which consider both qualitative and quantitative aspects of nutrition and physical activity in boys and girls with T2D, should remain inquiry and public health priorities.
Abbreviations
- BMI:
-
body mass alphabetize
- HbA1c:
-
glycated hemoglobin
- Kg:
-
kilogram
- L:
-
liter
- mtwo :
-
metres squared
- mmol:
-
millimole
- NIDDK:
-
Plant of Diabetes and Digestive and Kidney Diseases
- STOPP-T2D:
-
Studies to Treat Or Prevent Pediatric Type 2 Diabetes
- TODAY:
-
Handling Options for blazon 2 Diabetes in Adolescents and Youth
- T2D:
-
type 2 diabetes
- VLCD:
-
very-depression-calorie diet
- QI:
-
quality index
- QOL:
-
quality of life
References
-
American Diabetes Clan: Blazon 2 Diabetes in children and adolescents. Diabetes Care. 2003, 23: 381-389. 10.2337/diacare.23.3.381.
-
Writing Grouping for the SEARCH for Diabetes in Youth Report Group, Dabelea D, Bell RA, D'Agostino RB, Imperatore One thousand, Johansen JM, Linder B, Liu LL, Loots B, Marcovina S, Mayer-Davis EJ, Pettitt DJ, Waitzfelder B: Incidence of diabetes in youth in the Usa. JAMA. 2007, 297: 2716-2724. x.1001/jama.297.24.2716.
-
SEARCH for Diabetes in Youth Study Grouping, Liese AD, D'Agostino RB, Hamman RF, Kilgo PD, Lawrence JM, Liu LL, Loots B, Linder B, Marcovina Southward, Rodriguez B, Standiford D, Williams DE: The burden of diabetes among U.Southward. youth: prevalence estimates from the SEARCH for Diabetes in Youth Study. Pediatrics. 2006, 118: 1510-1518. ten.1542/peds.2006-0690.
-
Sinha R, Fisch M, Teague B, Tamborlane WV, Banyas B, Allen K, Savoye Yard, Rieger Five, Taksali Due south, Barbetta G, Sherwin RS, Caprio South: Prevalence of impaired glucose tolerance among children and adolescents with marked obesity. Northward Engl J Med. 2002, 346: 802-810. 10.1056/NEJMoa012578.
-
Fagot-Campagna A, Pettitt D, Engelgau M, Burrows Northward, Geiss L, Gregg Due east, Williamson D, Venkat Narayan K: Blazon two diabetes among North American adolescents: An epidemiologic health perspective. J Pediatrics. 2000, 136: 664-672. 10.1067/mpd.2000.105141.
-
Pavkov ME, Bennett PH, Knowler WC, Krakoff J, Sievers ML, Nelson RG: Issue of youth-onset type 2 diabetes mellitus on incidence of finish-stage renal disease and mortality in young and heart-aged Pima Indians. JAMA. 2006, 296: 421-426. 10.1001/jama.296.4.421.
-
Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, Nathan DM, Diabetes Prevention Program Research Group: Reduction in the incidence of type two diabetes with lifestyle intervention or metformin. N Engl J Med. 2002, 346: 393-403. ten.1056/NEJMoa012512.
-
Pan XR, Li GW, Hu YH, Wang JX, Yang WY, An ZX, Hu ZX, Lin J, Xiao JZ, Cao HB, Liu PA, Jiang XG, Jiang YY, Wang JP, Zheng H, Zhang H, Bennett PH, Howard BV: Effects of nutrition and practise in preventing NIDDM in people with dumb glucose tolerance. The Da Qing IGT and Diabetes Study. Diabetes Care. 1997, twenty: 537-544. ten.2337/diacare.xx.4.537.
-
Tuomilehto J, Lindström J, Eriksson JG, Valle TT, Hämäläinen H, Ilanne-Parikka P, Keinänen-Kiukaanniemi S, Laakso M, Louheranta A, Rastas M, Salminen V, Uusitupa M, Finnish Diabetes Prevention Study Grouping: Prevention of blazon two diabetes mellitus by changes in lifestyle among subjects with dumb glucose tolerance. North Eng J Med. 2001, 344: 1343-1350. 10.1056/NEJM200105033441801.
-
Look Ahead Research Grouping: Reduction in weight and cardiovascular illness risk factors in individuals with type two diabetes: ane-yr results of the look Ahead trial. Diabetes Care. 2007, xxx: 1374-1383. x.2337/dc07-0048.
-
Gillies CL, Abrams KR, Lambert PC, Cooper NJ, Sutton AJ, Hsu RT, Khunti 1000: Pharmacological and lifestyle interventions to forestall or delay type ii diabetes in people with impaired glucose tolerance: systematic review and meta-analysis. BMJ. 2007, 334: 299-10.1136/bmj.39063.689375.55.
-
American Diabetes Association: Blazon two Diabetes in Children and Adolescents: Consensus Statement. Diabetes Care. 2000, 23: 381-389. x.2337/diacare.23.iii.381.
-
American Diabetes Association: Standards of Medical Care in Diabetes - 2010. Diabetes Care. 2010, 33 (s1): S11-S61.
-
Canadian Diabetes Clan Clinical Practice Guidelines Expert Committee: Type 2 diabetes in children and adolescents. Tin can J Diabetes. 2008, 32 (s1): S162-S167.
-
Aslander-van Vliet East, Smart C, Waldron South: ISPAD Clinical Practice Consensus Guidelines 2006-2007. Nutritional management in childhood and adolescent diabetes. Pediatr Diabetes. 2007, eight: 323-339. 10.1111/j.1399-5448.2007.00317.x.
-
Robertson Yard, Adolfsson P, Riddell MC, Scheiner G, Hanas R: ISPAD Clinical Exercise Consensus Guidelines 2006-2007. Exercise in children and adolescents with diabetes. Pediatr Diabetes. 2008, nine: 65-77. x.1111/j.1399-5448.2007.00362.x.
-
Pinhas-Hamiel O, Zeitler P: Clinical presentation and treatment of type 2 diabetes in children. Pediatr Diabetes. 2007, 8 (S9): 16-27. 10.1111/j.1399-5448.2007.00330.10.
-
Libman I, Arslanian S: Prevention and treatment of type 2 diabetes in youth. Horm Res. 2007, 67: 22-34. 10.1159/000095981.
-
Downs SH, Blackness North: The feasibility of creating a checklist for the assessment of the methodological quality both of randomized and non-randomised studies of healthcare interventions. J Epidemiol Comm Wellness. 1998, 52: 377-384. ten.1136/jech.52.6.377.
-
Zdravkovic 5, Daneman D, Hamilton J: Presentation and course of Blazon 2 Diabetes in youth in a big multi-ethnic city. Diabet Med. 2004, 21: 1144-1148. 10.1111/j.1464-5491.2004.01297.x.
-
Grinstein Thou, Muzumdar R, Aponte Fifty, Vuguin P, Saenger P, DiMartino-Nardi J: Presentation and v-yr follow-upwardly of type 2 diabetes mellitus in African-American and Caribbean area-Hispanic adolescents. Horm Res. 2003, 60: 121-126. 10.1159/000072523.
-
Zuhri-Yafi MI, Brosnan PG, Hardin DS: Treatment of blazon 2 diabetes mellitus in children and adolescents. J Pediatr Endocrinol Metab. 2002, 15 (s1): 541-546.
-
Rothman RL, Mulvaney Southward, Elasy TA, VanderWoude A, Gebretsadik T, Shintani A, Potter A, Russell WE, Schlundt D: Self-management behaviors, racial disparities, and glycemic control amid adolescents with type 2 diabetes. Pediatrics. 2008, 121: e912-919. ten.1542/peds.2007-1484.
-
Reinehr T, Schober E, Roth CL, Wiegand Due south, Holl R: Type ii Diabetes in children and adolescents in a 2-Year follow-Upwardly: Insufficient adherence to diabetes centers. Horm Res. 2008, 69: 107-113. x.1159/000111814.
-
Shield JPH, Lynn R, Wan KC, Haines L, Barrett TG: Management and one twelvemonth event for UK children with type two diabetes. Arch Dis Child. 2009, 94: 206-209. 10.1136/adc.2008.143313.
-
Allan CL, Flett B, Dean HJ: Quality of life in first nation youth with type 2 diabetes. Matern Child Wellness J. 2008, 12: S103-S109. 10.1007/s10995-008-0365-ten.
-
Anderson One thousand, Dean H: The result of nutrition and practice on a native youth with poorly controlled non-insulin dependent diabetes mellitus. Beta Release. 1990, 14: 105-106.
-
Nichol H, Retallack J, Panagiotopoulos C: Cooking for your life! A family unit-centred, community-based nutrition educational activity program for youth with type 2 diabetes or impaired fasting glucose. Can J Diabetes. 2008, 32: 29-36.
-
Willi SM, Martin Thousand, Datko FM, Brant BP: Handling of Type 2 Diabetes in childhood using a very-low-calorie nutrition. Diabetes Care. 2004, 27: 348-353. x.2337/diacare.27.ii.348.
-
Kaufman FR: Type two diabetes in children and young adults: a "new epidemic.". Clin Diabetes. 2002, 20: 217-218. 10.2337/diaclin.20.4.217.
-
Bloomgarden ZT: Type 2 diabetes in the young: the evolving epidemic. Diabetes Intendance. 2004, 27: 998-1010. ten.2337/diacare.27.4.998.
-
Rosenbloom AL, Joe JR, Immature RS, Winter WE: Emerging epidemic of type ii diabetes in youth. Diabetes Care. 1999, 22: 345-354. 10.2337/diacare.22.2.345.
-
Goran MI, Davis J, Kelly L, Shaibi One thousand, Spruijt-Metz D, Soni SM, Weigensberg M: Depression prevalence of pediatric type 2 diabetes: where'southward the epidemic?. J Pediatr. 2008, 152: 753-755. ten.1016/j.jpeds.2008.02.004.
-
TODAY Report Group, Zeitler P, Epstein L, Grey M, Hirst Thou, Kaufman F, Tamborlane Westward, Wilfley D: Treatment options for type 2 diabetes in adolescents and youth: a study of the comparative efficacy of metformin lone or in combination with rosiglitazone or lifestyle intervention in adolescents with type 2 diabetes. Pediatr Diabetes. 2007, viii: 74-87. 10.1111/j.1399-5448.2007.00237.10.
-
Sinha I, Jones L, Smyth RL, Williamson PR: A systematic review of studies that aim to decide which outcomes to measure in clinical trials in children. PLoS Med. 2008, 29: five:e96-
-
Franks Pow, Hanson RL, Knowler WC, Moffett C, Enos 1000, Infante AM, Krakoff J, Looker HC: Childhood predictors of young-onset type 2 diabetes. Diabetes. 2007, 56: 2964-2972. 10.2337/db06-1639.
-
Zylke JW, DeAngelis CD: Child and boyish health--a call for papers. JAMA. 2008, 300: 2062-10.1001/jama.2008.606.
-
Golan M: Parents as agents of change in babyhood obesity - from research to practise. Int J Pediatr Obes. 2006, 1: 66-76. 10.1080/17477160600644272.
-
Norris C, Zhang 10, Avenell A, Gregg E, Bowman B, Serdula Thousand, Brown T, Schmid C, Lau J: Long-term effectiveness of lifestyle and behavioral weight loss interventions in adults with type ii diabetes: A meta-analysis. Am J Med. 2004, 117: 762-774S. 10.1016/j.amjmed.2004.05.024.
-
Tanofsky-Kraff M, McDuffie JR, Yanovski SZ, Kozlosky One thousand, Schvey NA, Shomaker LB, Salaita C, Yanovski JA: Laboratory assessment of the nutrient intake of children and adolescents with loss of control eating. Am J Clin Nutr. 2009, 89: 738-745. 10.3945/ajcn.2008.26886.
-
Reinehr T, Hebebrand J, Friedel S, Toschke AM, Brumm H, Biebermann H, Hinney A: Lifestyle intervention in obese children with variations in the melanocortin iv receptor factor. Obesity. 2009, 17: 382-389.
-
Pott Due west, Albayrak O, Hebebrand J, Pauli-Pott U: Treating childhood obesity: family unit background variables and the child's success in a weight-command intervention. Int J Eat Disord. 2009, 42: 284-289. 10.1002/eat.20655.
-
Brennan L, Walkley J, Fraser SF, Greenway 1000, Wilks R: Motivational interviewing and cognitive behaviour therapy in the treatment of adolescent overweight and obesity: study design and methodology. Contemp Clin Trials. 2008, 29: 359-375. 10.1016/j.cct.2007.09.001.
-
Schneider M, Hall WJ, Hernandez AE, Hindes K, Montez G, Pham T, Rosen L, Sleigh A, Thompson D, Volpe SL, Zeveloff A, Steckler A, HEALTHY Study Group: Rationale, pattern and methods for process evaluation in the HEALTHY study. Int J Obes. 2009, 33: S60-S67. 10.1038/ijo.2009.118.
Pre-publication history
-
The pre-publication history for this newspaper can be accessed here:http://www.biomedcentral.com/1471-2431/10/97/prepub
Acknowledgements
STJ, MC, JB, and TT-KH received no external back up. PWF is supported by Västerbotten's Health Say-so (ALF strategic date 2006-2009), the Swedish Heart-Lung Foundation (20070633), and the Swedish Diabetes Association (DIA2006-013). ASN is supported by a Career Development Award from the Canadian Child Health Clinician Scientist Program (funded by the Canadian Institutes of Health Research [CIHR]). GDCB is supported by a Population Wellness Investigator Laurels from Alberta Innovates - Health Solutions and a New Investigator Award from CIHR. These study sponsors did non play any role in this enquiry or in the conclusion to submit the paper for publication. Contents of the publication do not necessarily represent the views or policies of the National Institutes of Health.
Author information
Affiliations
Corresponding writer
Boosted information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
STJ contributed to written report pattern, data collection, brainchild and interpretation, drafted the kickoff manuscript and fabricated subsequent revisions. ASN conceived the report, made substantial contributions to the study blueprint and made disquisitional revisions of early on manuscript versions. MC participated in information collection and data abstraction. JB adult the search strategy and conducted the literature search. TTKH, PWF and MMJ provided critical revisions to the manuscript and provided important intellectual contributions. GDCB conceived the study, helped to solidify the study design and interpretation of data, drafted critical revisions, and, as did all authors, approved the terminal version of the manuscript.
Electronic supplementary textile
Authors' original submitted files for images
Rights and permissions
Open Access This article is published under license to BioMed Cardinal Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in whatsoever medium, provided the original work is properly cited.
Reprints and Permissions
About this article
Cite this article
Johnson, S.T., Newton, A.S., Chopra, M. et al. In search of quality evidence for lifestyle direction and glycemic control in children and adolescents with blazon 2 diabetes: A systematic review. BMC Pediatr x, 97 (2010). https://doi.org/10.1186/1471-2431-x-97
-
Received:
-
Accepted:
-
Published:
-
DOI : https://doi.org/ten.1186/1471-2431-10-97
Keywords
- Glycemic Control
- Lifestyle Modification
- Good Glycemic Command
- Pediatric Weight Direction
- Quality Index Score
lagrangealses1994.blogspot.com
Source: https://bmcpediatr.biomedcentral.com/articles/10.1186/1471-2431-10-97
0 Response to "Type 2 Diabetes in Children Peer Review Sources"
Post a Comment